Projects
About
Contact us

If you have useful clincial information from cases or simulation, please CLICK HERE to submit.
These scenarios are intended to help guide practice OR be used for simulation. They are based on insights from COVID-19 simulation / experience from managing other infectious diseases.
COVID-19
PRACTICAL GUIDANCE
CONTENTS
Click to download protocol for Emergency Drills in COVID-19 positive patient
Click to download transfer to theatre checklist
PERSONAL PROTECTIVE EQUIPMENT (PPE)
PERSONAL PROTECTIVE EQUIPMENT (PPE) in patients with confirmed / suspected COVID-19 infection
Public Health England and the RCOG have provided advice on what PPE should be used in different circumstances for patients who are confirmed / suspected COVID-19 positive. This advice is subject to change depending on changing evidence and experience.
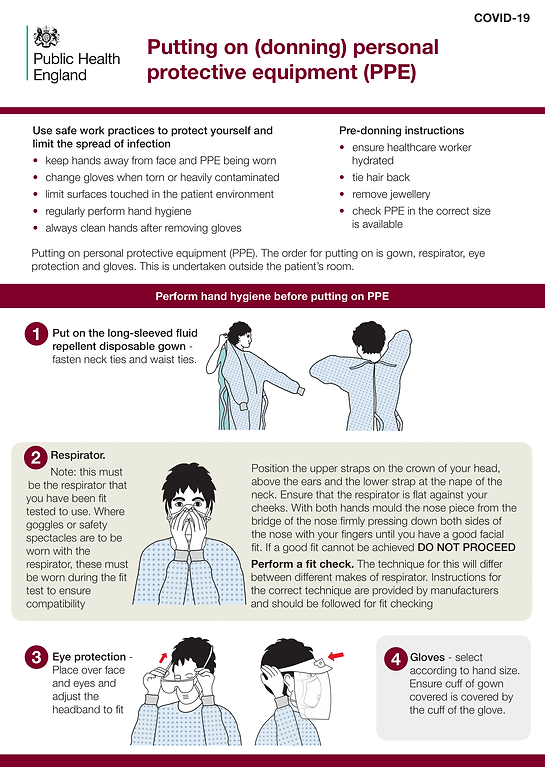
The main insight from a recent review of the evidence behind PPE from the Centre for Evidence Based Medicine (CEBM) is that PPE is a COMPLEX INTERVENTION and careful attention to should be paid to each aspect especially the donning and doffing. Doffing is arguably the more risky of the two because this is when contamination can potentially occur. Therefore staff should be especially careful when TAKING OFF PPE.
What is the evidence for PPE? (1 page)
ROUTINE WORK (WARD ROUNDS, CLINICS, EXAMINATIONS CLINICAL REVIEWS)
Patient wears mask
Staff wear:
1. PLASTIC APRON - Ideally with LONG sleeves
2. WATERPROOF MASK (normal surgical mask)
4. VISOR / EYE PROTECTION (Discretion if feels high risk of splash)
5. GLOVES (non-sterile)
When reviewing an unwell patient who is coughing / bleeding or where there is a risk of contact with other bodily fluids - use PPE as per labour below (wear visor + gown).
WOMEN IN LABOUR / CLOSE CONTACT PROCEDURES IN O&G (outside theatre)
The RCOG recognises that labour may increase the risks associted with transmission of COVID-19 due to contact with bodily fluids and the increased droplet generation that occurs due to increased maternal exertion. It is therefore recommended that staff wear a gown in addition to an apron. Public Health England do not however consider labour an 'Aerosol Generating Procedure' therefore an FFP3 (filtering face piece) mask is not routinely recommended. The exception to this is certain emergencies (where CPR is required and when a GA is required (see below).
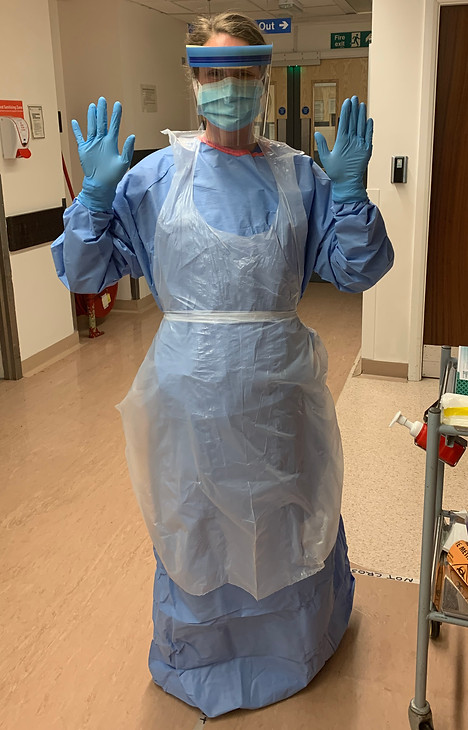
Attending a woman in labour (inclduing instrumental delivery in the room / suturing) staff wear:
1. GOWN
2. APRON (over gown)
3. VISOR / EYE PROTECTION
4. WATERPROOF MASK (normal surgical mask)
5. GLOVES (sterile or non-sterile depending on situation)
THEATRE CASES
Surgery/ theatre cases, where no intubation expected:
Staff should wear Full PPE and can remain in theatre during the regional anaesthetic:
1. STANDARD SURGICAL MASK
2. VISOR / EYE PROTECTION
2. SCRUB AS USUAL
3. GOWN
4. STERILE GLOVES
Any theatre case, even when done under regional anaesthesia can require intubation hence the requirement for a FFP3 mask.
Surgery/ theatre cases, GA/intubation required:
Full PPE, don in scrub room, must exit and be outside during intubation
1. FFP3 MASK
2. VISOR / EYE PROTECTION
2. SCRUB AS USUAL
3. GOWN
4. STERILE GLOVES
EMERGENCIES
Performing CPR is considered an Aerosol Generating Procedure. Intubation is also an AGP. When called to emergencies where either of these may be required, USE FULL PPE (as per labour) PLUS FFP3 MASK. Do not undertake emergency care including CPR without full PPE.

DONNING (putting on) and DOFFING (taking off) PPE advice from UK Govt

SETTING UP SOURCE ISOLATION
SETTING UP SOURCE ISOLATION
KEY PRINCIPLES
-
A minimal of 1 DONNING station (to put on PPE) and 2 DOFFING stations (to take off PPE) are required to look after suspected / confirmed COVID-19 patient.
-
The stations should have enough space to allow BUDDYING to take place.
-
A 2 METRE EXCLUSION ZONE should be made clear around areas of potential infection - the room where the patient is and the doffing station.

Donning station with area clearly marked for adequate buddying space not obstructing the passage of people / beds. Eqiupment in place for different levels of PPE as above - in case of emergency.
Handwashing & PPE donning instructions clearly visible above the station.

First doffing station inside room for staff to remove apron, gown and gloves. A double-bagged infectious waste bin should be available for these with alcohol for hand washing.
Staff leave mask and visor in situ before exiting the room.

Second doffing station outside the room. Infectious waste bin for mask and visor. Alchohol gel to clean hands after mask removal. Ideally should be reasonably close to a sink / changing room where staff can wash hands and change clothes if necessary.
In addition to marking around station, mark 2 metres either side so staff know where to avoid while others are removing PPE.
COMMUNICATION

In maternity services, like other high-risk areas of healthcare, staff are used to being able to communicate rapidly, often by moving in and out of rooms. Due to the highly contagious nature of COVID-19 and limitations of PPE, it is important to use other means of rapid communication such as 2-way radios (walkie talkies).
Some of the benefits of this are:
-
Reduced movement through isolation rooms.
-
Ability to rapidly communicate information to team outside allowing them to prioritise which staff should enter room / what eqiupment is required.
-
Staff inside room feeling less isolated and alone.

Other practical issues to consider:
-
Who should hold the walkie talkies in addition to the team inside the room? Suggestions include: most senior resident O&G doctor, Anaesthetist, Band 7 midwife, member of theatre team.
-
Develop or use a pre-existing standard system of communication, especially for emergencies.
-
Think about where the devices will be stored and how they will be cleaned.
-
Ensure that one walkie talkie remains outside the room at all times.
EMERGENCIES
Managing an Obstetric Emergency in a patient who is COVID-19 positive poses significant challenges in terms of balancing the need for urgent intervention with preventing staff from becoming infected.
4 KEY LESSONS FROM OBSTETRIC EMERGENCY SIMULATION IN A COVID-19 POSITIVE PATIENT:
-
EFFECTIVE USE OF PERSONAL PROTECTIVE EQUIPMENT IS THE PRIORITY. Whilst the instinct of staff may be to rush into an emergency disregarding their own safety, putting on Personal Protective equipment should be prioritised. Staff who become infected due to ineffective use of PPE will put themselves at personal risk. This will also have knock-on effects on the safety of the overall system if large numbers of staff are unable to attend work.
-
MANAGEMENT DELAYS ARE HIGHLY LIKELY in COVID-19 positive patients due to the need for staff to put on Personal Protective Equipment. Even in the context of emergencies (including cardiac arrest), staff are not to approach patients, commence management or enter isolation area without PPE which has been checked by a buddy. Removing PPE should also be done with a buddy.
-
EFFECTIVE USE OF BUDDY SYSTEM CAN GET SENIOR STAFF INTO ROOM QUICKLY. A donning system whereby three people put on PPE together and prioritise getting the most senior member of staff ready first, can get someone into the room much faster - 2 mins or less.
-
RAPID, EFFECTIVE COMMUNICATION IS ESSENTIAL such as using radio communication instead of phones and bleeps to minimise the delays introduced by the infection control, PPE requirements and increased cognitive load that will be borne by staff caring for COVID-19 patients.
In the senarios below, we simulated staff donning full PPE with FFP3 masks. It is important to note that the guidance around PPE is changing regularly so although this may not be the exact PPE required for each emergency, the key principles are the same - PPE must be prioritised and put on correctly before entering the room.
What this video demonstrates well, is just how long it takes to don PPE, even under controlled conditions, especially when first starting.
For the staff in the room, those minutes wiating for the team may seem like a very long time, therefore effective radio communication so that they know help is on the way, is crucial.
The timings opposite show how the process can be sped up if the buddy system is used differently, donning as trio instead of a duo. This is what happens in the next video. Even though the team are still learning to doff, the process happens much faster.

Finally, after the adrenaline and emotion of an emergency, it is important for staff to also remove the PPE with caution. One of the riskiest times in terms of infection risk is taking the visor off, therefore clearly marked and acessible doffing stations should be placed in close proximity to all areas where COVID-19 positive patients are cared for and staff should pay close attention to this part of the drill during simulation.
TRANSFER TO THEATRE
Based on experience from simulation and emerging clinical experience we have found that transferring patients to theatre in the context of suspected COVID-19 can be a complicated mulit-step process. We have therefore developed a checklist to help the team remember all of the steps.
Click to download transfer to theatre checklist


